Osseointegration: The Australian Experience After 500 Surgeries
By William Lu, PhD; Seamus Thomson; Jiao Jiao Li, PhD; Iana Wong; Calina Betlazar-maseh; and Munjed Al Muderis, MB ChB, FRACS, FAOrthA
There is no doubt that an amputated limb can have a dramatic and detrimental effect on patients and their families. Unfortunately, amputations are estimated to occur at a rate of 1.5 per 1,000 people, equivalent to a worldwide amputee population of more than 10 million.1
Amputations can occur due to traumatic accidents, tumors, malformations at birth, or even infection. When an amputation involves a lower limb, the mobility of the patient can be greatly limited, which may result in wheelchair confinement. The common solution for lower-limb amputees to regain function and mobility is to use an artificial leg that can restore some functionality of the lost limb.
Thanks to modern advancements in biomechanics and robotic engineering, we have seen vast improvements in artificial limb designs in recent years. A wide range of prosthetic options are currently available on the market, ranging from hydraulic polycentric knee joints that help reduce energy expenditure, to advanced bionic leg systems that are programmed to assist the patient’s gait through a complex array of algorithms and microprocessing power.2 It is thus not surprising for people to believe that the current prosthetics could completely replace the missing body parts and fully restore mobility. However, the personal experiences of lower-limb amputees and their families tell us that the solutions available today are still far from ideal, and many patients are still challenged to perform even the simplest daily activities.
Problems With Current Prostheses
The major problem lies in the way that these robotic limbs are attached to the body. For more than six centuries, the main method to attach a limb prosthesis was through a socket-mounted system.3 A socket is essentially a custom-shaped bucket that is designed to wrap around and append to the residual limb by means of pressure, grip, or vacuum suction on the soft tissue (skin, muscles, and fat). One can easily imagine the amount of stress exerted on the skin, especially when full body weight is constantly loaded onto the limb. As a result, patients using socket prostheses often suffer from chronic skin problems, such as discomfort, sweating, heat, and chafing due to friction, skin ulcerations, and pain.4
Apart from the many issues related to discomfort, socket prostheses have a number of other crucial drawbacks as well. Because socket prostheses attach mechanical limbs to the body through layers of soft materials (e.g., fabric and silicone liners), the many layers involved in this attachment not only reduce patients’ ability to precisely control the leg position, but they also largely dampen the sensory feedback required for the patient to sense the ground and walk with confidence. Despite the improvements in modern artificial limbs, their functionality and practicality are still greatly restricted by these drawbacks of the traditional socket system.
Development and Advantages of Osseointegration
In 1965, Professor Per-Ingvar Brånemark invented the modern dental implant by threading transoral titanium implants into the bones of the upper and lower jaw to act as anchorage for dental prostheses.5 This invention sparked the modern concept of “osseointegration,” which essentially means biomechanically integrating artificial biomaterials with the living bone.
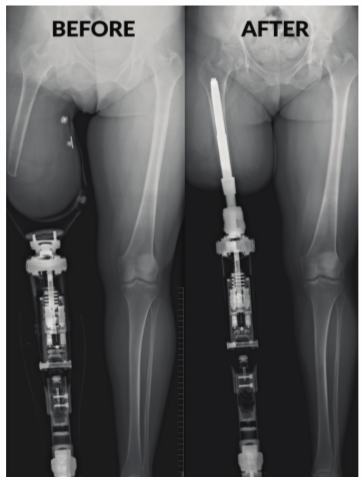
Based on this concept, in the early 1990s the first transcutaneous femoral prosthesis was implanted on an above-knee amputee.6 Instead of using a socket to adhere to the body through layers of soft tissue, osseointegration inserts a metal implant directly into an amputee’s residual bone, with the distal end passing through the skin, which connects to an artificial limb system (see Figure 1). This technology provides a rigid and intimate biomechanical connection that directly loads the amputee’s skeletal system, which would reduce bone resorption if not enhance bone formation. It also allows the patient to restore proprioception (feeling of the ground); increase motion of the hip; increase ability to control the prosthetic limb; benefit from greater comfort during sitting and standing; and experience easier donning and doffing, reduced pain levels, and overall better mobility and quality of life—these advantages basically circumvent all of the challenges caused by traditional socket design.
Safety Concerns
The idea of a piece of metal protruding through the limb may sound intimidating to some people. Understandably, the medical community in the early days raised concerns regarding infection risks among patients who received this type of surgery.
The Journal of Bone and Joint Surgery (JBJS) recently published an in-depth article that investigated the safety concerns of osseointegrated reconstruction in transfemoral amputees.7 Among 86 transfemoral amputees who had received an osseointegrated implant for more than two years in Australia, the study found that mild infection and irritation of the soft tissue in the skin-penetration area were common. However, the study also reported that these infections were usually minor and could be successfully managed with simple measures such as a single course of oral antibiotics. Moreover, the paper concluded that “severe infections resulting in septic implant loosening are rare.”
Overall, osseointegrated implants are becoming well-accepted among clinicians, with the belief that the infection risks are minor and manageable. Among the patients, it was found that the use of basic hygiene practices, such as daily showering and routine cleaning of the skin-penetration area, can keep the infection risks at a lower level.8
Introduction of The Osseointegration Group
of Australia
In the last few years, with the introduction of modern techniques of anchoring the skin to the bone and moving away from a two-stage to a single-stage surgery, Professor Munjed Al Muderis, MB ChB, FRACS, FAOrthA, from Sydney, Australia, has successfully converted the osseointegration technology from a niche procedure for a selected number of patients to a popular intervention that can be applied to a wider population of amputees. This technique has dramatically reduced the time needed for rehabilitation, the risks of infection, and other complications. Osseointegration for amputees has now become a standard method of treatment in this population.
Currently, there are only a few clinics in the world offering the pioneering technology of osseointegration to amputees. It is estimated that around 1,000 procedures have been performed worldwide. One of the largest clinical groups offering the procedure is The Osseointegration Group of Australia, led by Al Muderis. The Australian team has performed over 500 osseointegration cases to date. It adopts a multidisciplinary approach with expert input from surgeons, pain specialists, anesthetic and rehabilitation specialists, physiotherapists, prosthetists, psychologists, nursing staff, engineers, and clinical researchers on each individual case. This multidisciplinary structure allows the team to address challenging cases ranging from the femur, tibia, and humerus, to the radius, including extremely short residuums and complex cases.
Moreover, the Australian team also is the first center to perform osseointegration in a single-stage surgery, which can reduce the total rehabilitation period to as short as three to six weeks.9 The improvement is largely due to a newly designed press-fit Osseointegrated Prosthetic Limb (OPL) implant that achieves interlocking bony ingrowth in a relatively short period of time. The new implant contrasts with the original screw-fixation devices, which require a two-stage surgical procedure with a total rehabilitation time of six to eight months before a patient can ambulate without walking aids. In addition, this refined single-stage approach reduces a patient’s exposure to risks of complications, with a noticeable reduction in the number of elective soft-tissue refashioning surgeries and the overall infection rate.
Further Advantages
Importantly, the experience from The Osseointegration Group of Australia offers insight into many of the clinical challenges commonly observed in the field. The surgical risks and complication rates for above-knee amputees is now comparable to common joint arthroplasty procedures. In Australia, to date, there have been no femoral osseointegration implants removed due to infection, and the revision rate for a femoral single-stage osseointegration surgery is currently below 1.5 percent.
Traditionally, patients with amputations due to peripheral vascular disease (PVD) or diabetes have been excluded from this surgery. However, a recent study published by the Australian team has shown that osseointegration may conversely provide a restorative effect against the progression of the underlying diseases among these patients.10 Moreover, other studies investigating bone mineral density changes have demonstrated significant advantages through the direct loading of the residual bone, which reversed the risks of severe osteoporosis commonly observed in long-term socket users (see Figure 2).
In addition, customized 3-D-printed titanium implants enabled the team to reconstruct amputations beyond the femur, with more than 140 transtibial cases and several transhumeral, transradial, and digital cases performed. Furthermore, the multidisciplinary team has successfully combined limb lengthening technology with osseointegration to reconstruct extremely short (<5-cm) bony residuums. Recent breakthroughs in targeted muscle reinnervation (TMR) surgery have demonstrated promising results in pain reduction as well as enabled advanced functional control for upper-limb amputees.11
Recognition and Future Development
Having gone through significant improvements in implant design, surgical technique, and rehabilitation protocols, osseointegrated limb reconstruction has come a long way since it was first performed more than 30 years ago. Osseointegration is now considered a safe and effective method of limb reconstruction that can restore the functionality of a lost limb as close as possible to normality.
By combining osseointegration and TMR technology, amputees nowadays are able to regain their mobility without enduring common problems caused by the traditional socket and enjoy a life with reduced pain and greater prosthetic control.
So far, only two osseointegration devices have been approved in Europe, Australia, and New Zealand, and are commercially available in these regions. Patient-specific devices and investigational device trials are currently underway in the United States and are showing promising results. It can be expected that approval by the U.S. Food and Drug Administration of these devices will take place within the next few years. Therefore, it appears that scientists and clinicians have found a suitable alternative to replace sockets as a preferred method of prosthetic attachment.
Osseointegration not only offers new hope to the millions of amputees for regaining mobility and improving their quality of life, but also represents a huge step toward the future development and application of advanced bionic prostheses.
William Lu, PhD; Seamus Thomson; Jiao Jiao
Li, PhD; Iana Wong; Calina Betlazar-maseh;
and Munjed Al Muderis, MB ChB, FRACS, FAOrthA, are part of the Clinical Research Team at The Osseointegration Group of Australia.
References
- Dillingham TR, Pezzin LE, MacKenzie EJ. Limb Amputation and Limb Deficiency: Epidemiology and Recent Trends in the United States. Southern Medical Journal. 2002 Aug; 95(8):875-883.
- Hafner BJ, Willingham LL, Buell NC, Allyn KJ, Smith DG. Evaluation of Function, Performance, and Preference as Transfemoral Amputees Transition From Mechanical to Microprocessor Control of the Prosthetic Knee. Archives of Physical Medicine and Rehabilitation. 2007 Feb 1; 88(2):207-217.
- Thurston AJ. Paré and Prosthetics: The Early History of Artificial Limbs. ANZ Journal of Surgery. 2007 Dec 1; 77(12):1114-1119.
- Meulenbelt HE, Dijkstra PU, Jonkman MF, Geertzen JH. Skin Problems in Lower-Limb Amputees: A Systematic Review. Disability and Rehabilitation. 2006 Jan 1; 28(10):603-608.
- Brånemark PI. Osseointegration and Its Experimental Background. The Journal of Prosthetic Dentistry. 1983 Sep 1; 50(3):399-410.
- Hagberg K, Brånemark R. One Hundred Patients Treated With Osseointegrated Transfemoral Amputation Prostheses—Rehabilitation Perspective. J Rehabil Res Dev. 2009 May 1; 46(3):331-344.
- Al Muderis M, Khemka A, Lord SJ, Van de Meent H, Frölke JP. Safety of Osseointegrated Implants for Transfemoral Amputees: A Two-Center Prospective Cohort Study. JBJS. 2016 Jun 1; 98(11):900-909.
- Hebert JS, Rehani M, Stiegelmar R. Osseointegration for Lower-Limb Amputation: A Systematic Review of Clinical Outcomes. JBJS Reviews. 2017 Oct 1; 5(10):e10.
- Al Muderis M, Lu W, Tetsworth K, Bosley B, Li JJ. Single-Stage Osseointegrated Reconstruction and Rehabilitation of Lower-Limb Amputees: The Osseointegration Group of Australia Accelerated Protocol-2 (OGAAP-2) for a Prospective Cohort Study. BMJ Open. 2017 Mar 1; 7(3):e013508.
- Atallah R, Li JJ, Lu W, Leijendekkers R, Frölke JP, Al Muderis M. Osseointegrated Transtibial Implants in Patients With Peripheral Vascular Disease: A Multicenter Case Series of Five Patients with One-Year Follow-Up. JBJS. 2017 Sep 20;99(18): 1516-1523.
- Kuiken TA, Li G, Lock BA, Lipschutz RD, Miller LA, Stubblefield KA, Englehart KB. Targeted Muscle Reinnervation for Real-Time Myoelectric Control of Multifunction Artificial Arms. JAMA. 2009 Feb 11; 301(6):619-628.
Figure 1
Osseointegration involves inserting a metal rod directly into an amputee’s residual bone, with the distal end exiting the skin, which then attaches to an artificial limb system.
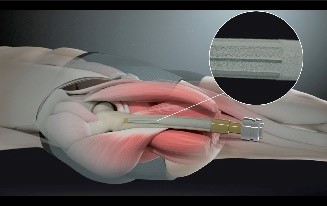
Figure 2
Osseointegration enables the direct loading of the residual limb (right), while in the traditional socket-mounted prosthesis the residual limb can easily deviate from the mechanical axis (left). This deviation results in severe limitations in functional control while the nonloading of the residual bone also can lead to severe osteoporosis.